



Marrow Cellution
Bone Marrow Harvesting Systems
Marrow Cellution
Bone Marrow Harvesting Systems
Aspirate to Application without Centrifugation
Bone Marrow Aspirate collected with the Marrow Cellution™ System has shown a dramatic increase in key stem and progenitor cells when compared to centrifugated marrow from leading systems.
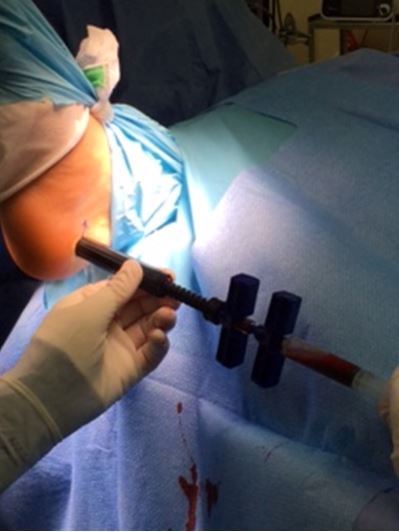
The patent pending Marrow Cellution™ System maximizes the yield of stem and progenitor cells by giving the clinician the ability to efficiently harvest bone marrow from multiple levels within the medullary space, while restricting dilution caused by peripheral blood.
Marrow Cellution™ and A Functional Bone Matrix: The Power of Synergy

Overview
Overview
Limitations of Traditional Needles
Traditional bone marrow aspiration needles aspirate primarily through an open-ended cannula, which leads to excess peripheral blood dilution and inadequate collection of key stem and progenitor cells. For this reason a high volume of bone marrow aspirate must be collected and then manipulated (i.e. centrifuged) before being utilized for regenerative therapies.
Jamshidi needles were designed to draw very small volumes from multiple insertion points. This technique was subsequently modified by limiting the insertion points and drawing larger volumes (60-240 mL). The aspirate was then reduced through centrifugation due to peripheral blood dilution. This technique delivers low numbers of fibroblastic-like stem cells and is often augmented with expensive allograft alternatives to complete the biologic profile for tissue regeneration.
Overcoming Limitations with Marrow Cellution
The patent pending Marrow Cellution™ System overcomes the limitations of a traditional bone marrow needle by allowing the user to aspirate in a measured and controlled manner over a large geography inside the marrow space, while restricting peripheral blood infiltration.
Two unique design features are the key:
The closed-tip aspiration cannula restricts aspiration through the side holes of the cannula and away from the channel caused by the tip of the needle, avoiding excess peripheral blood infiltration.
A mechanical means for measured and controlled retraction of the aspiration cannula allows the clinician to collect marrow aspirate from multiple geographies inside the medullary space with a single puncture.
Reduce the Cost of Utilizing Biologics
The Marrow Cellution™ System delivers a better regenerative solution at a reduced cost compared to the industry leading alternatives.
Minimize O/R Time
Centrifugation systems typically required 20 minutes or more of spin time during the surgical procedure, not to mention the additional support time needed for preparation and cleanup of the equipment.
Minimize Sterility Challenges
Centrifugation systems require passing the BMA off the sterile field for processing, and back on for implantation. The Marrow Cellution™ System eliminates the additional steps where infection concerns must be managed.
Minimize Sample Waste
Centrifugation systems typically discard 80% of the aspirate due to high levels of peripheral blood. Worse, significant numbers of the desired cells (approx. 40%) are discarded because as these cells increase in density prior to division, they are processed into the undesired red cell centrifuge component and thus discarded, substantially limiting the regenerative potential of the resulting sample.
Minimize Use of Anti-Coagulants
Centrifugation systems require at least 10% dilution by volume for the addition of anti-coagulant to allow the sample to separate, and also require another 10% dilution in the form of a neutralizing agent such as thrombin and calcium chloride in order for the marrow to clot in the graft. The Marrow Cellution™ System eliminates these requirements.
Eliminate the Need to Filter
Protocols require the marrow to be filtered prior to centrifugation. Cells bound within a clot cannot be counted but they can be delivered to the patient when mixed with graft material or injected. This is not the case when clots are filtered out prior to centrifugation. Filtering takes additional time, but more importantly, filtering reduces regenerative potential.

Competition
Competition
Comparing CFU-F per mL
Comparing published results from the leading BMAC competitors against independent real-world clinical usage of the Marrow Cellution™ System demonstrated overwhelming superiority in regenerative potential, as measured by CFU-F per mL.
Why use CFU-F count?
CFU-F (Colony Forming Unit - Fibroblast) counts are the established metric for measuring the regenerative potential of bone marrow. TNC (total nucleic cell) counts include nucleated red blood cells and white blood cells from the peripheral blood component of the aspirate which have little regenerative capability. Published research consistently use CFU-F counts to identify the thresholds for clinical efficacy.
Resources
Resources
Head to Head Analysis
These analyses explore sets of bone marrow aspirate samples that were collected during surgery from bilateral iliac crest draws with different BMAC systems and the Marrow Cellution system, each being randomly assigned to one iliac crest.
White Papers & Presentations
Marrow Cellution Bone Marrow Aspiration System and related concentrations of stem and progenitor cells (updated data set).
Below is an edited podium presentation by Dr. Michael Scarpone, presenting his findings along with Daniel Kuebler, PhD on using the Marrow Cellution device without centrifugation.
Updated paper by Dr. Joseph Purita titled Novel Technology to Increase Concentrations of Stem and Progenitor Cells in Marrow Aspiration. n = 27
Presentation comparing the data from using Marrow Cellution product to other techniques, including centrifugation.
FAQs
FAQs
DOES A SMALL VOLUME ASPIRATE HAVE MORE CFU-F THAN A LARGER DRAW THAT IS THEN VOLUME REDUCED BY CENTRIFUGATION?
In order to centrifuge marrow, you need to add 10% by volume anti-coagulant. This dilutes the end product. You do not need to add that volume of anti-coagulant if you are not centrifuging.
When you centrifuge marrow, approximately 40% of the stem cells are discarded with the red cells. Stem cells / progenitor cells when they are cycling build up nucleic mass prior to division. At this stage their density increases dramatically to the point where they have a similar density to a red cell. Centrifugation protocols capture a range of cells based on density. In any given aspirate, approximately 40% of the stem cells have density outside what is typically captured in the buffy coat.
Typically, the centrifugation protocol volume reduces the aspirate from 60cc to 10cc. This 10cc is then used to hydrate the substrate. However, in order to reverse the effect of the anti-coagualnt, to make the marrow clot, about 1cc of calcium chloride and thrombin is mixed with the concentrate; another 10% dilution.
Centrifuge does not distinguish between nucleated cell from marrow verses blood. So a sample may have a lot of nucleated cells but very few came from marrow. A CFU-f test is often performed on marrow aspirate because CFU-f are found in marrow but not blood.
Finally, there is no way to draw 60cc of marrow, no matter how careful, and not get significant peripheral blood dilution. A careful draw of 60cc with multiple punctures typically, at best, gets on average 300 cfu-f per mL.
The math play for a typical centrifuged marrow aspirate sample plays out as follows.
| CFU-f per mL | 300 |
| volume | 60 mL |
| Total CFU-f per mL | 18,000 |
| Recovery in the concentrate | 60% |
| Total CFU-f in Concentrate | 10,800 |
| Concentrate Volume | 7 mL |
| CFU-f per mL | 1,543 |
| HSS / Hedge Study | 1,270 |
This compares to 2,000 CFU-f per mL drawn from a single site in the marrow.
Juopperi TA, Schuler W, Yuan X, Collector MI, Dang CV, Sharkis SJ. Isolation of bone marrow-derived stem cells using density-gradient separation. Experimental hematology 2007;35:335-41.
Bhartiya D, Shaikh A, Nagvenkar P, et al. Very small embryonic-like stem cells with maximum regenerative potential get discarded during cord blood banking and bone marrow processing for autologous stem cell therapy. Stem cells and development 2012;21:1-6.
Vishal Hegde MD et al; “Title: A prospective comparison of three approved systems for autologous bone marrow concentration demonstrated non-equivalency in progenitor cell number and concentration.” Journal of Orthopaedic Trauma Publish Ahead of Print
MUSCHLER G, et al “Aspiration to Obtain Osteoblast Progenitor Cells from Human Bone Marrow: The Influence of Aspiration Volume” The Journal of Bone and Joint Surgery; VOL. 79-A, NO. 11. Cleveland Clinic
Hernigou. P et al “Benefits of small volume and small syringe for bone marrow aspirations of mesenchymal stem cells” Int Orthop 2013 Nov;37 (11): 2279-87
WHAT ARE THE LIMITATIONS OF TRADITIONAL NEEDLES AND WHAT IS THE OPTIMAL TECHNIQUE FOR MINIMIZAING PERIPHERAL BLOOD DILUTION?
Optimal technique for minimizing peripheral blood with a traditional aspiration needle is to perform a single small volume pull (2 mL) from the distance most proximal from the entry of the needle. Larger volumes of bone marrow aspirate contain higher amounts of peripheral blood because the cannula is open ended and because traditional needles do not have a mechanical means for precise relocation. Aspirating after retracting the needle exacerbates the problem of peripheral blood contamination by exposing the open ended cannula to the resulting channel that is created by the needle itself and that is filled with peripheral blood.
These results confirmed that strict adherence to a specific collection procedure, involving small volume marrow aspirations and multiple puncture sites, results in a product with a high number of early hematopoietic progenitor cells and minimal contamination by peripheral blood.
Spitzer et al “The impact of harvest center on quality of marrows collected from unrelated donors.” J Hematother. 1994 Spring;3(1):65- 70. Massachusetts General Hospital, Boston 02114.
The data shows that as the aspiration volume increases from any one given site, the concentration of bone marrow derived cells decreases quickly and the fraction of the sample composed of peripheral blood increases.
MUSCHLER G, et al “Aspiration to Obtain Osteoblast Progenitor Cells from Human Bone Marrow: The Influence of Aspiration Volume” The Journal of Bone and Joint Surgery; VOL. 79-A, NO. 11. Cleveland Clinic
This study shows that marrow harvesting by means of multiple small volume aspirations minimizes the dilution with peripheral blood and results in greater numbers of cells and hemopoietic progenitors.
Bone marrow harvest for marrow transplantation: effect of multiple small (2 ml) or large (20 ml) aspirates. Bacigalupo A et al; Bone Marrow Transplantation. [1992, 9(6):467-470]
Aspirates of bone marrow demonstrated greater concentrations of mesenchymal stem cells with a 10-ml syringe compared with matched controls using a 50-ml syringe.
Int Orthop 2013 Nov;37 (11): 2279-87 Benefits of small volume and small syringe for bone marrow aspirations of mesenchymal stem cells Hernigou. P et al
A larger-volume of aspirate from a given site is contraindicated with the additional volume contributing little to the overall number of bone-marrow cells and results principally in unnecessary blood loss.
MUSCHLER G, et al “Aspiration to Obtain Osteoblast Progenitor Cells from Human Bone Marrow: The Influence of Aspiration Volume” The Journal of Bone and Joint Surgery; VOL. 79-A, NO. 11 Cleveland Clinic
WHAT ARE THE DIFFERENT TECHNIQUES TO ASPIRATE MARROW USING A TRADITIONAL NEEDLE AND WHAT CAN I EXPECT FOR CFU-F PER ML USING SUCH TECHNIQUES?
We are aware of four different protocols documented in the literature to aspirate greater than 1mL of bone marrow per puncture using a legacy needle. Legacy needle is defined as a standard open-ended trocar with side ports and a removable stylet. The techniques and the corresponding reported average number of cfu-f per mL is described below:
- Insert the needle and begin to aspirate from a single location (cfu-f 376 per mL; volume 10 ml : cfu-f 95 per mL ; volume 50 mL)
- Insert the needle further into the bone space and aspirate marrow in different locations as you retract the needle from the marrow space (cfu-f 356 per mL; volume 8 mL : cfu-f 52 per mL; volume 30 mL)
- Aspirate marrow using a standard BD 30mL syringe in different locations as you advance the needle into the marrow space by inserting the blunt stylet to advance the trocar to each new depth from which aspirate is taken (cfu-f 54 per mL; volume 30 mL)
- Aspirate marrow using a vacuum assisted (vac-lok merit medical) 30mL syringe in different locations as you advance the needle into the marrow space by inserting the blunt stylet for each new depth from which aspirate is taken. (cfu-f 205 per mL; volume 30 mL)
Of course, drawing 1mL always gave by far the most cfu-f per mL. (Between 1,500 -2,000 cfu-f per mL) Each additional unit of volume taken from the initial location became significantly contaminated with peripheral blood.
For volumes of aspirate greater than 1 mL, there was no benefit to moving the needle forward or backward or leaving it in one place. Sequentially larger volumes of aspirate were always associated with greater peripheral blood contamination. A benefit was achieved by controlling the amount of negative pressure through use of a vac-lok syringe at each staged location for the aspirate as the needle was advanced.
Technique 1 and 2 used a 10 mL syringe to aspirate 8-10mL of marrow, with the corresponding mean cfu-f counts being 376 and 356 per mL, respectively. Employing technique 1 and using a 50mL syringe to increase the negative pressure while drawing the 10 mL reduces the cfu-f mL to 180 mL. Employing technique 1 using a 50 mL syringe and increasing the aspirate volume to 50 mL from a single location reduces the cfu-f mL to 95. Employing technique number 2 to aspirate 30 mL with a standard 30 mL syringe produced 52 cfu-f mL. Employing technique 3 to aspirate 30 mL of aspirate using a standard 30 mL syringe resulted in 54 cfu-f per mL. Finally, employing technique 4 to aspirate 30 mL using a vacuum assisted syringe to control the negative pressure at each 5 mL stage as the needle is advanced resulted in 205 cfu-f per mL.
The results above demonstrate the effect of peripheral blood contamination associated with larger aspirations of marrow; specifically lower cfu-f per mL. The results outlined above are consistent with the body of scientific literature developed over the last 30 years supporting the use of marrow for pathology and oncology purposes.
McLain RF, Fleming JE, Boehm CA, Muschler GF. Aspiration of osteoprogenitor cells for augmenting spinal fusion: comparison of progenitor cell concentrations from the vertebral body and iliac crest. J Bone Joint Surg Am 2005;87:2655-61.
Hernigou p; et al. Benefits of small volume and small syringe for bone marrow aspirations of mesenchymal stem cells. Int Orthop. 2013 Nov;37(11):2279-87.
Muschler GF, Boehm C, Easley K. Aspiration to obtain osteoblast progenitor cells from human bone marrow: the influence of aspiration volume. J Bone Joint Surg Am 1997;79:1699-709.
Hegde V, Shonuga O, Ellis S, et al. A prospective comparison of 3 approved systems for autologous bone marrow concentration demonstrated nonequivalency in progenitor cell number and concentration. Journal of orthopaedic trauma 2014;28:591-8.
Jones et al; Rapid intraoperative concentraton of mesenchymal stem cells from bone marrow aspriate Spine Care, Houston TX; Biomet Inc.
WHAT IS THE IMPORTANCE OF CFU-F COUNTS COMPARED TO NUCLEATED CELL COUNTS?
There is no constant ratio between average marrow cellularity as measured by number of total nucleated cells per mL and the number of cfu-f. Hernigou et al in several authoritative studies linked clinical outcomes in non-union and osteonecrosis to the number of cfu-f cells in the graft. Controlling for volume, Hernigou et al noted that 70% of the variation in cfu-f from patient to patient was due to variations in the quality of the marrow aspirate or idiosyncratic to the patient with the remaining variation being due to the of number of nucleated cells per mL in the aspirate. Statistically, the only variable Hernigou reported to be significant was cfu-f and not nucleated cells per mL. Interestingly, cfu-f is found frequently in marrow and very rarely in peripheral blood. From Hernigou “Therefore, it seems reasonable to suggest that a graft needs to contain greater than 1000 progenitors / cm ^3”.
Hernigou et al Treatment of Osteonecrosis with autologous bone marrow grafting Clinical Orthopaedics and Realted Research number 405, pp 14-23
Hernigou P, et al Percutaneous Autologous Bone-Marrow Grafting for Nonunions – Influence of the Number and Concentration of Progenitor Cells The Journal of Bone and Joint” Volume 87-A No 7 July 2005
DO I NEED TO FILTER SPICULES FROM MARROW AFTER ASPIRATION AND ARE RED CELLS A PROBLEM?
Spicules:
Fragments, also known as spicules, are aggregates of bone marrow cells that are pulled from the bony matrix of the marrow space (trabecular) during the aspiration process. They represent what will be seen on the bone marrow biopsy as material that came from what was in between the bony trabecular. Many of these aggregates are smaller than 200 micron filter so, you are not filtering many of them out anyway but you do lose them with a centrifugation protocol. Typical filter is capturing fat and clots. Bone Chunks would not fit through the 22 gauge needle or the side ports of the aspiration needle. These cell aggregates are VERY rich in MSC and HSC. (1,2)
1) Ahmadeigi et al ;The aggregate nature of human mesenchymal stromal cells in native bone marrow. Cytotherapy 2012 Sep;14(8):917-24. 2) Ahmadbeigi et al Isolation, Characterization, and Transplantation of Bone Marrow Derived Cell Components with Hemtopoietic Stem Cell Niche Properties Stem Cells Dev. 2013 Dec 1; 22(23): 3052–3061.
RBC Count:
The hematocrit of the product from the needle will be the native hematocrit and will be equal to that of centrifugation protocols but will have a slightly higher number of nucleated red blood cells. Red cells are a natural part of any clot and play a role in the regenerative process; it is not necessary to remove them.
- Red cell are nitric oxide sinks ( ref 1)
- Nitric Oxide is a potent stem cell stimulant (ref 2)
- Red Cells release iron
- Iron is used by cells under stress to survive and function (ref 3)
- Stem cells reside deep in the red cell layer including very small embryonic-like cells are discarded during centrifugation . (ref 4, 5, 6)
1) Cortese et al Endothelial nitric oxide synthase in red blood cells: Key to a new erythrocrine function Volume 2, 2014 251-258 http://www.sciencedirect.com/science/article/pii/S221323171400010X
2) Alexandra Aicher Essential role of endothelial nitric oxide synthase for mobilization of stem and progenitor cells Nature Medicine 9, 1370 - 1376 (2003) Published online: 12 October 2003;
3) Gardner, et al Superoxide Radical and Iron Modulate Aconitase Activity in Mammalian Cells June 2, 1995 The Journal of Biological Chemistry, 270
4) Ahmadbeigi et al The aggregate nature of human mesenchymal stromal cells in native bone marrow. Cytotherpy 2012 Sep;14(8):917-24.
5) Juopperi et al Isolation of Bone Marrow Derived Stem Cells using Density-Gradient Separation Experimental Hematology 35 (2007) 335-341
6) Bhartiva D et al “Very Small Embryonic-Like Stem Cells with Maximum Regenerative Potential Get Discarded During Cord Blood Banking and Bone Marrow Processing for Autologous Stem Cell Therapy” Stem Cells and Development Volume 221 NO 1 2012
In Vivo Data:
Lastly, this established science corresponds to published in-vivo clinical experience where marrow of a native hematocrit was used to treat knee cartilage defects. No adverse reactions were noted when a native level of marrow cells was used. (1,2)
1) Gobbi A. Et al “One-Step Cartilage Repair with Bone Marrow Aspirate Concentrated Cells and Collagen Matrix in Full-Thickness Knee Cartilage Lesions; Results at 2-Year Follow-up” Cartilage. 2011 Jul; 2(3): 286–299A.
2) Fortier L. et al. “Concentrated Bone Marrow Aspirate Improves Full-Thickness Cartilage Repair Compared with Microfracture in the Equine Model” J Bone Joint Surg Am. 2010 Aug 18;92(10):1927-37
WBC Count:
When an aspirate is performed poorly ( i.e. single stick draw using a vac-syringe, aspirate all from one location) the aspirate is comprised mostly of peripheral blood. The density of the float in the marrow kits is greater than the PRP kits and so the BMAC kit will capture more red cells and granulocytes. In the case of a poor aspirate, the only difference between PRP and BMAC, since they are both being made from peripheral blood, is that the BMAC has higher red cells and granulocytes. With a poor aspirate, the higher nucleated cell counts in the centrifugation protocols is due to higher cells from the peripheral blood and not marrow cells. The published literature looks at the number of CFU-F in the marrow product, whether centrifuged or not, to determine the quality of the biologic because CFU-F is found in marrow but not peripheral blood. Clinical results in these peer reviewed journal articles for different muscular skeletal dis-orders were lined to CFU-F in the graft, not the nucleated cell content.
Centrifugation / Concentration:
Many cell aggregates from the marrow aspirate are as dense as a mature red cell. (1,2) This is the reason why centrifugation protocols get such a low percent recovery of mesenchymal stem cells (CFU-F); they are thrown away with the red cells. Quote from ref 3 below: “The isolated cells from both the upper and lower fractions were characteristic of MSC. Although it is commonly believed that MSC are single suspending mononuclear cells and so are enriched in the upper fraction of Ficoll-Paque after density-gradient separation, our data showed that considerable numbers of these cells were accumulated in the lower fraction.” (3) Lastly, whole blood is used for epidural patches; if red cells were inflammatory, they could not be used near such sensitive tissues.
1) Juopperi TA, Schuler W, Yuan X, Collector MI, Dang CV, Sharkis SJ. Isolation of bone marrow-derived stem cells using density-gradient separation. Experimental hematology 2007;35:335-41.
2) Bhartiya D, Shaikh A, Nagvenkar P, et al. Very small embryonic-like stem cells with maximum regenerative potential get discarded during cord blood banking and bone marrow processing for autologous stem cell therapy. Stem cells and development 2012;21:1-6.
3) Bhartiva D et al “Very Small Embryonic-Like Stem Cells with Maximum Regenerative Potential Get Discarded During Cord Blood Banking and Bone Marrow Processing for Autologous Stem Cell Therapy” Stem Cells and Development Volume 221 NO 1 2012
IS THERE A RELATIONSHIP BETWEEN DIFFERING VOLUMES OF BONE MARROW ASPIRATES AND THEIR CELLULAR COMPOSITION?
A dramatic decline in the number of HSC and CFU-f is observed with increasing amounts of marrow aspiration. With respect to HSC and in the setting of large volume aspirations (1,000 mL and greater) for allogeneic transplantation, the first 1mL of marrow had 3X (300%) more nucleated cells and 10X (1000%) more stem cells than the overall aspirate. Similarly, it has been documented that the number of MSC per/mL significantly decreases with increased volumes of aspirate taken.
Importantly, the number of CFU-f in incremental aspirations of over 100 mL have as little as 60 CFU-f / mL.
Batinic, D et al “Relationship between differing volumes of bone marrow aspirates and their cellular composition.” Bone Marrow Transplant. 1990 Aug;6(2):103-7.
Jing Li; et al “Factors Affecting Mesenchymal Stromal Cells Yield from Bone Marrow Aspiration” Chin J Cancer Res. Mar 2011; 23(1): 43–48.
MUSCHLER G, et al “Aspiration to Obtain Osteoblast Progenitor Cells from Human Bone Marrow: The Influence of Aspiration Volume” The Journal of Bone and Joint Surgery; VOL. 79-A, NO. 11, NOVEMBER 1997
Vishal Hegde MD et al; “Title: A prospective comparison of three approved systems for autologous bone marrow concentration demonstrated non-equivalency in progenitor cell number and concentration.” Journal of Orthopaedic Trauma Publish Ahead of Print
WHAT IS THE RELATIONSHIP BETWEEN AGE AND ASPIRATION QUALITY FOR BONE MARROW?
1) the cellularity of marrow declines with age
2) the cellularity of marrow per / mL declines with increasing aspiration volumes.
Muschler G et al “Age- and gender-related changes in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors” Journal of Orthopaedic Research Volume 19, Issue 1, pages 117–125, January 2001 Pang W et al “Human bone marrow hematopoietic stem cells are increased in frequency and myeloid-biased with age” PNAS vol. 108 no. 50 20012–20017
WHAT IS THE IMPORTANCE OF CD34 COMPARED TO NUCLEATED CELL COUNTS?
The hematopoietic colony-forming cell content of the transplant is associated more rigorously with the major covariates of success than is the total nucleated cells and is, therefore, a better index of the content of grafts.
Migiacciao AR et al “Cell dose and speed of engraftment in placental/umbilical cord blood transplantation: graft progenitor cell content is a better predictor than nucleated cell quantity.” Blood: 2000 Oct 15;96(8):2717-22.
DOES THE NUMBER OF CD34+ CELLS IN MARROW DECLINE WITH AGE?
It has been documented that the number of nucleated cells per/mL of marrow aspirate declines with age as red marrow is replaced with fatty marrow. (7) However, the ratio of CD 34 cells to nucleated cells remains constant or increases with age. (8) Consequently, the overall number of CD 34 cells declines with age and is correlated with age-associated declines in the nucleated cell content of the marrow.
Muschler G et al “Age- and gender-related changes in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors” Journal of Orthopaedic Research Volume 19, Issue 1, pages 117–125, January 2001 Pang W et al “Human bone marrow hematopoietic stem cells are increased in frequency and myeloid-biased with age” PNAS vol. 108 no. 50 20012–20017
WHAT HAS BEEN REPORTED FOR THE NUMBER OF CD34+ CELLS PER ML FROM ASPIRATES STRATIFIED BY AGE?
| Age | Sample # | Volume | MNC X10^6 | MNC / mL | CD34 | CD34 / mL |
|---|---|---|---|---|---|---|
| 0-20 | 35 | 92 | 434 | 4,717,391 | 1.05% | 49,532.61 |
| 21-40 | 203 | 100 | 403 | 4,030,000 | 1.04% | 41,912.00 |
| 41-60 | 83 | 100 | 367 | 3,670,000 | 0.94% | 34,498.00 |
| 61-80 | 11 | 100 | 302 | 3,020,000 | 0.93% | 28,086.00 |
Vidyasagar et al “Index of CD34+ Cells and Mononuclear Cells in the Bone Marrow of Spinal Cord Injury Patients of Different Age Groups: A Comparative Analysis” Bone Marrow Research Volume 2012
DO THE NUMBER OF CFU-F CELLS IN MARROW DECLINE WITH AGE?
It has been documented that the number of nucleated cells per/mL of marrow aspirate declines with age as red marrow is replaced with fatty marrow. However, the ratio of CFU-f to nucleated cells remains constant for men but declines for postmenopausal women. Consequently, the overall number of CFU-f cells declines with age for both men and women and is correlated with age associated declines in the nucleated cell content of the marrow. However, such declines are more precipitous for postmenopausal women.
Muschler G et al “Age- and gender-related changes in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors” Journal of Orthopaedic Research Volume 19, Issue 1, pages 117–125, January 2001
DOES THE OVERALL HEALTH OF THE PATIENT POPULATION HAVE AN INFLUENCE ON THE NUMBER OF CD34+ CELLS?
The following table summarizes the number of Total Nucleated Cell (TNC) and CD 34+ / mL from different patient populations: 1) pre-screened allogeneic marrow donors, 2) commercial sources of marrow where by donors and samples are pre-screened and discarded if a certain number of cells are not present.
| Source | TNC / mL | CD 34 / mL |
|---|---|---|
| Scheduled for Cardiac Surgery | 9.8 | 49,000 |
| Allogeneic Marrow Donor | 17.7 | 125,670 |
| Purchased Marrow for Research | 23.5 | 136,764 |
Donnenberg AD et al; “Intra-operative preparation of autologous bone marrow-derived CD34-enriched cellular products for cardiac therapy.” Cytotherapy. 2011 Apr;13(4):441-8.
McKenna, DH et al “CD34+ Cell Selection Using Small Volume Marrow Aspirates: A Platform for Novel Cell Therapies and Regenerative Medicine” Cytotherapy. Apr 2010; 12(2): 170–177
DO CERTAIN LIFESTYLE CHOICES IMPACT THE NUMBER OF CD34+ CELLS & CFU-F IN THE MARROW?
Conditions such as alcohol abuse, smoking, lack of exercise and a poor diet are associated with fewer numbers of CD34+ cells and cfu-f in the marrow.
Hernigou et al Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002 Dec;(405):14-23. Alexander Mackie PhD CD34-Positive Stem Cells in the Treatment of Heart and Vascular Disease in Human Beings Tex Heart Inst J. 2011; 38(5): 474–485.
DO CERTAIN MEDICATIONS IMPACT THE NUMBER OF CD34+ CELLS & CFU-F IN THE MARROW?
Statins are associated with a dramatic and dose dependent increase in the number of CD34 cells in both the marrow and in circulation. Corticosteriod use is associated with impaired cellularity of the marrow space and osteonecrosis of the hip. Bisphosphanate use is associated with osteonecrosis of the jaw.
Dimmeler et al; HMG-CoA reductase inhibitors (statins) increase endothelial progenitor cells via the PI 3-kinase/Akt pathway J Clin Invest. 2001 Aug 1; 108(3): 391–397. Hernigou et al Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002 Dec;(405):14-23. Marx et al Bisphosphonate-Induced Exposed Bone (Osteonecrosis/Osteopetrosis) of the Jaws: Risk Factors, Recognition, Prevention, and Treatment Journal of Oral and Maxillofacial Surgery Volume 63, Issue 11, November 2005, Pages 1567–1575
DO CERTAIN DISEASES IMPACT THE NUMBER AND/OR FUNCTIONALITY OF CD34+ CELLS & CFU-F IN THE MARROW?
Sickle cell disease and diabetes are known to impact the marrow space. In the case of sickle cell disease, the marrow space tends to be hyper-active and marrow aspirates from these patients are associated with higher numbers of CD 34 and cfu-f. In the case of diabetes, the functionality of the marrow cells is significantly impaired.
Hernigou et al Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002 Dec;(405):14-23. Tepper et al Human endothelial progenitor cells from type II diabetics exhibit impaired proliferation, adhesion, and incorporation into vascular structures. Circulation [2002, 106(22):2781-2786]
WHAT IS THE PURPOSE OF CENTRIFUGATION PROTOCOLS FOR MARROW?
To compensate for peripheral blood dilution due to with increasing volumes of aspiration from a single location within the marrow space, clinicians have used centrifugation protocols to volume reduce 50 to 60 mL of aspirate to 7 to 10 mL by removing excess plasma and red blood cells from the peripheral blood. The final treating composition typically has a concentration above baseline of nucleated cells from the peripheral blood and the marrow.
MUSCHLER G, et al “Aspiration to Obtain Osteoblast Progenitor Cells from Human Bone Marrow: The Influence of Aspiration Volume” The Journal of Bone and Joint Surgery; VOL. 79-A, NO. 11, NOVEMBER 1997 Vishal Hegde MD et al; “Title: A prospective comparison of three approved systems for autologous bone marrow concentration demonstrated non-equivalency in progenitor cell number and concentration.” Journal of Orthopaedic Trauma Publish Ahead of Print
WHAT IS THE IMPACT OF AGE ON PERIPHERAL BLOOD PLATELETS AND VASCULOGENESIS?
Platelets and white blood cells from peripheral blood are essential to healing and the body naturally aggregates platelets and white cells efficiently to sites of trauma. With age, your body does not lose its ability to aggregate platelets from blood to the area of a defect. Vasculogenesis (i.e. the ability of your body to mobilize stem cells from the marrow space to the site of trauma) does diminish significantly with age because of fewer stem cells in the body and a diminished ability to travel to sites of a defect. With age, marrow mediated healing diminishes dramatically. Transplanting marrow exactly mimics and supplements your body's critical response to healing, a response that diminishes with age.
Lommatzsch, M et al The impact of age, weight and gender on BDNF levels in human platelets and plasma. Neurology of Aging, January 2005 Volume 26, Issue 1, Pages 115–123 Heiss et al Impaired Progenitor Cell Activity in Age-Related Endothelial Dysfunction JACC Journal of American College of Cardiology; volume 45, Issue 9, May 2005 Scheubel et al Age-dependent depression in circulating endothelial progenitor cells inpatients undergoing coronary artery bypass grafting J Am Coll Cardiol. 2003;42(12):2073-2080.
CAN THE MARROW CELLUTION NEEDLE BE USED TO ASPIRATE FROM BONES OTHER THAN THE ILIAC CREST?
The body of scientific literature has documented that the ilicac crest and vertebral body are both rich sources of marrow aspirate, followed by the distal ends of long bones such as the tibia and calcaneus. The MC Ran 11 C can be used in the pedicle and the MC-RAN-11 and MC-RAN-8 can be used in the iliac crest as well as other bones such as the calcaneus or tibia. Since the tibia and calcaneus have fewer cells than the iliac crest, some clinicians supplement their bone grafts with a bone dowel from those sites as well as an aspirate using the MC-RAN-8 product. Bone dowels harvested in this manner can be delivered over a traditional 8 gauge needle to reduce the morbidity of transplanting or placing the graft into the defect site.
WHAT IS THE OPTIMAL SYRINGE PLUNGER TECHNIQUE AND SYRINGE SIZE TO OPTIMIZE THE RECOVERY OF MARROW DURING ASPIRATION?
Gronkjaer et al researched the question of whether a gentle pull of the syringe plunger or a rapid jerk of the plunger, creating a rapid negative pressure inside the syringe, made a difference in the recovery of cells. They determined that a rapid jerk-like motion of the plunger resulted in twice the number of cells compared to gently pulling the plunger. Intuitively this makes sense given the difference in viscosity between blood and marrow. A gentle pull allows the lower viscous blood to begin to flow leaving the higher viscous marrow in tact in the marrow. A rapid jerk of the plunger creates a larger pressure differential at the lumen openings of the needle inside the marrow space. This rapid pressure change does not give the blood a chance to seep into the needle ahead of the marrow.
Therefore, with the Marrow Cellution™ system, the approximate 1mL fill should be accomplished by rapidly jerking back the plunger. Each 1 mL fill is accomplished at each new location after turning the handle 360 degrees counter clockwise as the aspiration cannula is removed from the body using the screw set. The plunger should be let go after each additional 1 Ml fill. This will cause the pressure inside the syringe to normalize and therefore the plunger will automatically position itself at the fill line, which should be about 1 mL higher than the previous fill line.
Hernigou et al researched whether a larger syringe that creates a greater pressure differential will result in greater cells per mL. For varying volumes of aspirate, they compared a 10mL syringe to a 50mL syringe. They concluded that the optimal syringe size was 10mL combined with a rapid pull of the plunger optimizing the negative pressure. Their rationale for the results was that the resistance of pulling back the 10mL syringe was so much less than the larger syringe. Therefore, the user was able to create a more rapid change in pressure using the 10 mL syringe even though the larger 50 mL syringe was ultimately able to create a greater overall vacuum. Once the less viscous peripheral blood begins to flow, the higher vacuum of the 50 mL syringe worked at cross-purposes to capturing higher viscous marrow cells. They also reported, regardless of syringe size, that greater volumes of marrow from any one location resulted in fewer cells per mL due to infiltrating peripheral blood. Therefore, the optimal technique is to use a 10mL syringe with a rapid plunger motion and with a 1 mL draw from each location.
Therefore, with the Marrow Cellution™ system, we provide a 10 mL syringe and at each aspiration site, we teach to fill 1 mL to no more than 2 mL by pulling plunger back to maximum vacuum; release the plunger, move the needle and repeat the process until the needle has been unwound from the body.
Acta Haematologica , October 2016 135:81-87 Bone Marrow Aspiration: A Randomized Controlled Trial Accessing the Quality of Bone Marrow Specimens Using Slow and Rapid Aspiration Techniques and Evaluating Pain Intensity Gronkjaer et al
Int Orthop 2013 Nov;37 (11): 2279-87 Benefits of small volume and small syringe for bone marrow aspirations of mesenchymal stem cells Hernigou. P et al



